Abstract
Introduction: Guidelines from the American Society of Hematology recommend consideration of outpatient management, rather than hospitalization, for patients with pulmonary thromboembolism (PTE) with low risk of complication. The simplified Pulmonary Embolism Severity Index (sPESI) is frequently used for PTE risk stratification and selection for outpatient management, where an sPESI of 0 is associated with a low risk of recurrent thromboembolism, non-fatal bleeding, and death. Prior to developing an outpatient care pathway for low risk PTE at a large, public academic medical center, we sought to assess the potential clinic volume by determining the number of patients seen at our institution with low risk acute PTE. We also sought to capture other features that may preclude outpatient management including renal impairment, thrombocytopenia, and obesity, which may prevent direct oral anticoagulant (DOAC) use, and lack of insurance, which may impede access to affordable anticoagulation and clinic follow-up.
Methods: We retrospectively identified patients with acute PTE by reviewing computed tomography (CT) of the chest with contrast or CT angiography performed during a one-year period (Oct 1, 2018 to Sept 30, 2019) using CPT codes. Imaging reports were manually reviewed to determine if acute PTE was present. sPESI variables were collected: age >80, history of cancer, history of cardiopulmonary disease, heart rate (HR) ≥110bpm, systolic blood pressure (SBP) <100mmHg, and oxygen saturation (O 2) <90%. Medical history variables were identified using ICD-10 codes. Vital sign values were determined by identifying peak or nadir as appropriate within 24 hours of encounter initiation. Additional demographic and clinical variables collected included sex, weight, body mass index (BMI), insurance status, serum creatinine, platelet count, and length of stay for admitted patients. Readmission was determined by reviewing documentation within 30 days of initial encounter. Values were reported using frequencies with percentages and means with standard deviation and/or range. Comparisons were performed using chi squared tests and t tests as appropriate.
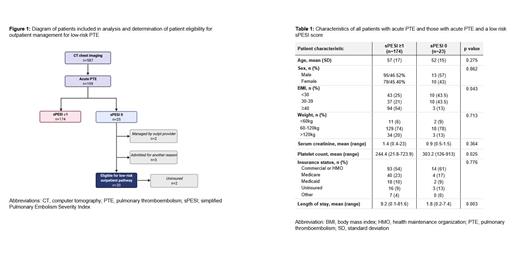
Results: Of 587 CT chest imaging studies identified, 199 (34%) demonstrated acute PTE (Figure 1). The majority (n=174, 87%) had an sPESI of 1 or greater. Points were more frequently gained due to SBP <100mmHg (n=109, 63%), HR ≥110bpm (n=105, 60%), and O 2 ≤90% (n=90, 52%). History of cancer was present in 54 patients (31%) and history of cardiopulmonary disease in 81 patients (47%), with a total of 113 patients (65%) having a history of either. Only 25 patients (13%) had a low risk sPESI score of 0. Two patients with sPESI of 0 were excluded from further analysis due to age <18 and transfer to an outside hospital. Table 1 includes a comparison of the demographic and clinical features of all patients with acute PTE versus those with sPESI of 0.
Of those patients with a low risk sPESI, 3 patients (13%) had another indication for hospital admission aside from acute PTE (Figure 1). Three patients (13%) had a BMI greater than 40kg/m 2 and a weight greater than 120 kilograms. No patients had significant renal impairment, with a serum creatinine ranging between 0.5-1.5mg/dL. No patients had significant thrombocytopenia. Three patients (13%) were uninsured, 1 of whom was admitted for another indication.
The majority of patients with sPESI of 0 were admitted (n=19, 83%) with an average length of stay of 1.8 days (SD 1.6, range 0.2-7.4). Two patients were discharged from the emergency department (ED), and 2 patients were diagnosed and managed by an outpatient provider without contact with the ED or hospital. Only 1 patient was readmitted to the hospital within 30 days for reasons unrelated to PTE.
Conclusions: Our results indicate that the annual volume for a low risk PTE outpatient management pathway at a large, public medical center would be low, with only 20 patients meeting eligibility per sPESI in 12 months. Patients were frequently disqualified for vital sign abnormalities, but over half were ineligible due to comorbidities. This quantification will allow our institution and others that are similar to gauge the potential resource allotment needed for low risk pathway development. In addition, we demonstrate that 10% of eligible patients were uninsured, emphasizing that access to affordable anticoagulation and follow-up is necessary when developing outpatient PTE care models.
No relevant conflicts of interest to declare.